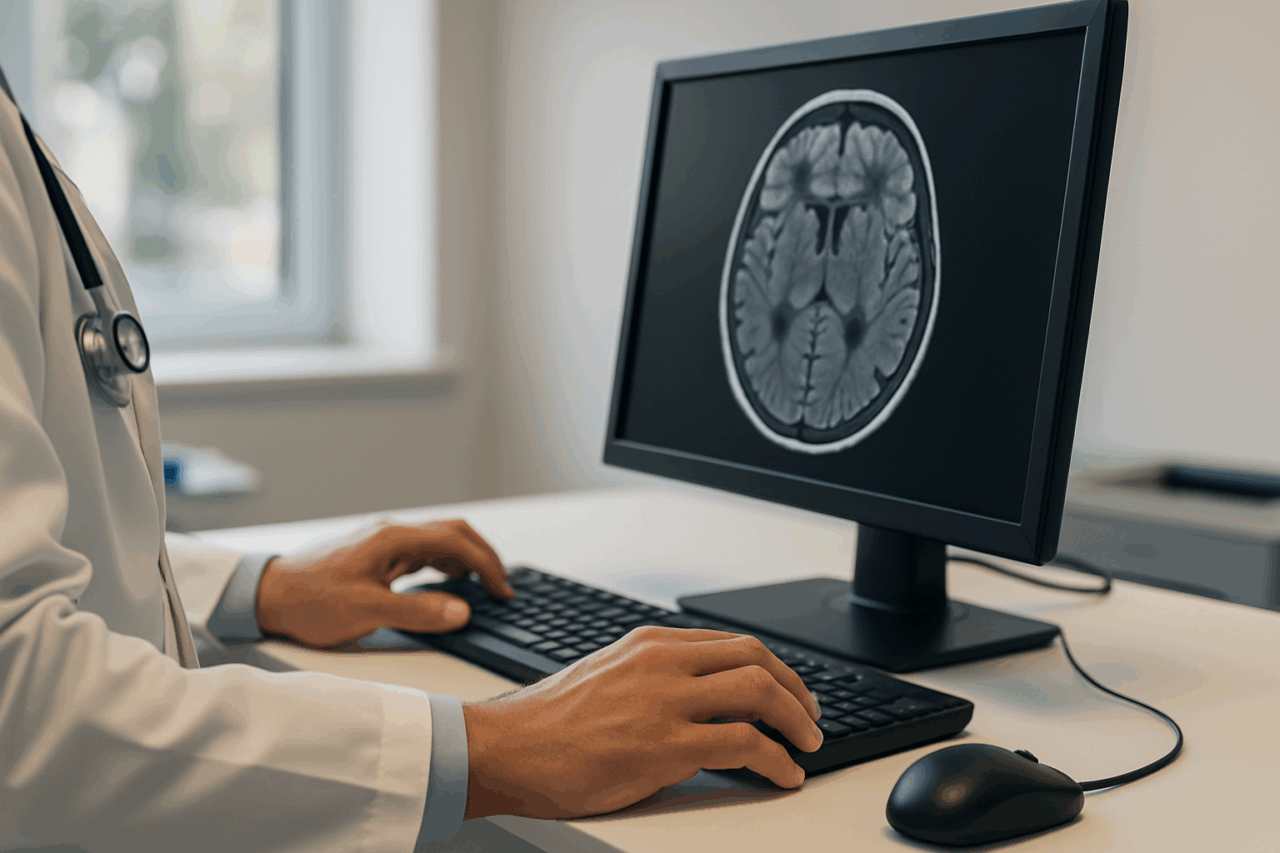
Surgery Can Now Start in the Scanner
A common frustration in congenital cardiology is that the most consequential decisions still depend on piecing together partial views. Echocardiography excels at real-time valve motion but can be constrained by acoustic windows and angle dependence. CT provides crisp anatomy but cannot directly visualize flow and brings ionizing radiation into a population likely to need repeated imaging across a lifetime. Cardiac MRI can measure flow and tissue without radiation, yet clinical teams have often had to choose between images that show structure well and images that show hemodynamics well.
February 16, 2026
Illustration 30114332 © Krishnacreations | Dreamstime.com
February 5, 2026
ID 147819612 | Background © Yota Nik | Dreamstime.com
February 5, 2026
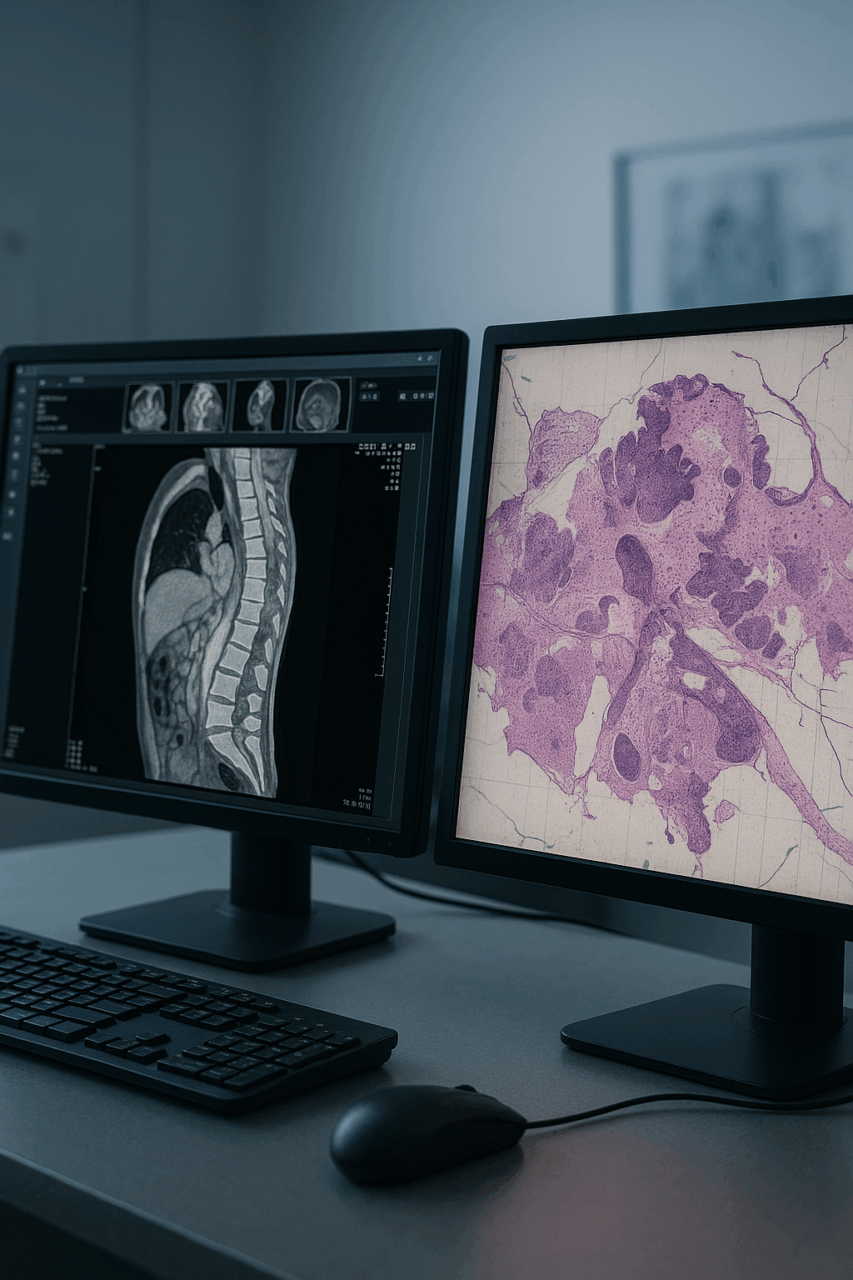
Photo 178859620 | Cancer © Mr.phonlawat Chaicheevinlikit | Dreamstime.com
January 26, 2026
ID 209680455 © Transversospinales | Dreamstime.com
Mount Sinai: AI That Asks Its Own Questions Could Transform Clinical Diagnostics
October 20, 2025
A human face and a glowing AI face connect through circuitry, symbolizing harmony between human cognition and artificial intelligence in healthcare.
AI Order Creation Tools Are Gaining Speed, but Not Yet Trust
February 5, 2026
Photo 130409802 | Ai © Funtap P | Dreamstime.com
The Interface Architect: The Most Powerful People You’ve Never Heard Of in Healthcare IT
June 11, 2025
Breach Remediation Is Not Security
February 16, 2026
ID 187020383 © Josepalbert13 | Dreamstime.com
Mount Sinai’s CHIME Digital Maturity Signals the Next Phase of AI-Driven Care Delivery
December 22, 2025
courtesy of The Mount Sinai Health System
Surgery Can Now Start in the Scanner
February 16, 2026
Illustration 30114332 © Krishnacreations | Dreamstime.com
TEFCA’s Strategic Crossroads: Governance, Payment Levers, and the Real Market Reordering
May 12, 2025
Health Systems Must Prepare for the Operational Reality of Social Needs Screening
December 2, 2025
Photo 94227568 | Healthcare © Pop Nukoonrat | Dreamstime.com
Telehealth Secured, PBMs Scrutinized in Latest Spending Bill
February 5, 2026
ID 147819612 | Background © Yota Nik | Dreamstime.com
SYNERGEN Health’s Sunil Konda Explores AI’s True Role in Revenue Cycle Strategy
July 15, 2025
Photo 137404548 | Healthcare © Nuthawut Somsuk | Dreamstime.com