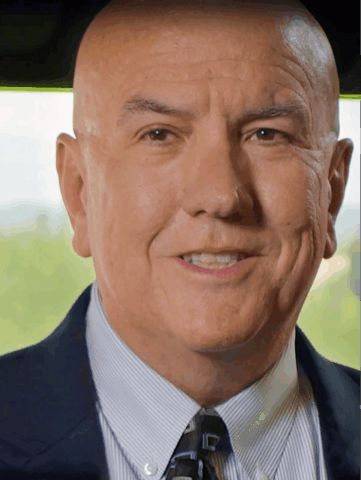
Kent Dick, CEO, Life365
As healthcare systems grapple with staffing shortages, financial pressure, and widening access disparities, virtual care is infrastructure. Yet for many organizations, the promise of remote care has been undermined by fragmented platforms, clinician burnout, and inconsistent patient engagement. Kent E. Dicks, CEO of Life365, believes the next era of digital health will be defined not by more apps or devices, but by seamless, invisible systems that fit into clinicians’ workflows and patients’ lives without disruption.
In this interview, he shares how automation, AI, and design simplicity are converging to make proactive, personalized, and equitable care a reality. For CIOs, CMIOs, and digital health strategists navigating the next phase of virtual care, Dicks lays out a model rooted in usability, data intelligence, and systemic impact.
You’ve described the goal of making virtual care technology “invisible.” What does that mean in practical terms for clinicians and patients, and why is it so important?
“Invisible” virtual care technology means tools and systems that work seamlessly in the background, without creating friction for clinicians or patients. For clinicians, it means receiving clear, actionable insights within their existing workflows – without the need to sift through excessive data or learn new software. For patients, it means intuitive, automated devices that don’t require frequent manual input or troubleshooting. This invisibility is crucial because complexity leads to disengagement, while simplicity fosters sustained use, better care coordination, and improved health outcomes. The key in this conversation is data, which AI/Machine Learning systems need to surveil large populations of patients to determine those likely to head to the ED/hospital and try to head that off in advance. Doctors don’t need more data; what they need is an intelligent platform like AI with which they can work in partnership to move to proactive, predictable, personalized and prioritized care.
Clinician burnout is at an all-time high, with EHR demands and data overload often cited as major contributors. How can health systems reduce this burden while still scaling virtual care programs?
To reduce burnout while scaling virtual care, health systems must prioritize automation and usability. That includes integrating EHRs with AI-driven tools that filter data into actionable insights and eliminate unnecessary administrative work. Systems should aim to deliver the right information at the right time – during patient interactions – rather than overwhelming clinicians with raw data. By simplifying workflows and offloading routine tasks, clinicians can focus more on care and less on documentation. I often equate the role of a newer automobile to healthcare. Currently, cars have analyzers that tell exactly where trouble may be happening. Data plays an important role for providers in a similar manner to help point out issues and trends that might be important for consideration, especially occurring outside the traditional healthcare setting – home.
What steps can healthcare leaders take to ensure remote patient monitoring (RPM) programs are equitable and effective for older adults and rural populations?
Leaders must tailor virtual care programs to the specific needs of their patient populations. This includes accounting for tech literacy, infrastructure limitations, and access to in-person support. For example, rural and older patients often require additional technical assistance. Programs should be piloted with a single condition before scaling and must offer alternative support channels, like community liaisons or hybrid in-person visits, to bridge digital gaps and ensure no group is left behind. In our recent heart failure studies, we found that our older patients were more comfortable with cellular devices (scales, blood pressure, etc.) that come out of the box ready to use, automatically connecting to the network – no configuration, versus using an “app” on their smart phones that connects to Bluetooth devices, which resulted in more complication in downloading and pairing, and a poor user experience.
You’re quoted as saying that data must become actionable insights. How can automation and AI help turn raw patient data into meaningful, preventive care interventions?
Automation and AI can analyze large volumes of patient data in real time and surface only what matters most – such as missed screenings or signs of health deterioration. These tools enable clinicians to move from reactive to proactive care. For example, rather than combing through reports manually, clinicians receive targeted recommendations during patient interactions. This allows them to intervene early, prevent hospitalizations, and reduce avoidable costs. In addition, data helps with the personalization of the connected solution to help maximize patient engagement, on their terms, while providing valuable insights into a patient’s condition to help with prioritization and intervention on those that could be headed to the ED/hospital. Data and AI play an important role in surveilling a population of patients in a passive way. EHR/EMR data provides a wealth of information, along with claims data and genomics, to help train AI models of care for patient populations. Observational data on a near real-time basis also plays an important role in prioritization and intervention – by detecting breach of data patterns that led patients to the ED/hospital in the past.
For health systems looking to launch or refine a virtual care program, where should they start to avoid overwhelming their staff and patients?
The best starting point is a focused, phased approach. Rather than rolling out RPM for multiple conditions at once, begin with one high-priority chronic condition like hypertension. Build workflows that integrate smoothly with existing systems and tailor them to your community’s demographics. Success here builds momentum, staff confidence, and patient trust – creating a strong foundation to scale the program over time without overwhelming resources or users. Build the RPM/virtual care solution into the clinical workflow of the provider to make it seamless to order a patient to be put on remote care. This should help facilitate alignment of the right devices to collect the data, the shipping of devices to the patients, and the smooth integration of the data back into the patient’s record – all from the simple order that started in the EHR. Engagement also plays an important role for patients, so they can follow the providers’ instruments and take their readings on a regular basis, without the provider needing to intervene.
![Image: [image credit]](/wp-content/uploads/dreamstime_xxl_120537759-scaled.jpg)